Imagine you have just undergone parotid surgery, a procedure often necessary to remove tumors from the parotid gland, the largest of the salivary glands. Everything seemed fine until you started experiencing jaw pain after parotidectomy. You are not alone—many patients report similar concerns. As a leading head and neck oncologist in Mumbai, Dr. Devendra Chaukar has seen this issue firsthand. He is here to guide you through understanding what might be causing your discomfort and how it can be managed effectively.

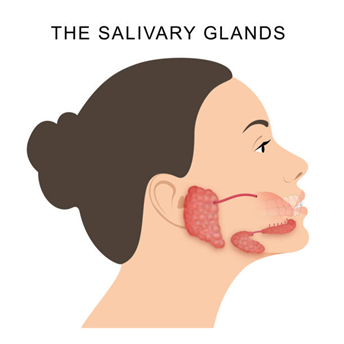
Yes, it is relatively common to experience jaw pain after parotidectomy. This discomfort often stems from nerve irritation or inflammation around the surgical site. The facial nerve, which runs through the parotid gland, can become irritated during the procedure, leading to pain or numbness. Furthermore, muscle stiffness and scar tissue formation can contribute to discomfort, particularly when moving the jaw.
Dr. Devendra Chaukar, an expert in parotid surgery in Mumbai, explains,
“Jaw pain after parotid surgery is not uncommon and usually resolves with proper postoperative care and time. Understanding the causes can help in managing the symptoms effectively.”
What are the causes of jaw pain after parotidectomy?

Jaw pain after a parotidectomy can arise from various factors related to the surgery itself and the body’s response to healing. Here are the key causes:
Nerve irritation or injury
The facial nerve, which controls movements of the face, passes through the parotid gland. During surgery, this nerve can be irritated or, in rare cases, injured. Even minor nerve irritation can cause discomfort, numbness, or pain in the jaw area.
Muscle stiffness and inflammation
First bite syndrome
First bite syndrome after parotidectomy is a specific type of pain that occurs when you take your first bite of food. It is characterized by intense pain in the jaw or near the ear, triggered by salivary gland stimulation. This occurs due to nerve damage or changes in the autonomic nerves that regulate the salivary glands.
Scar tissue formation
As the surgical area heals, scar tissue can form around the area where the parotid gland was removed. This scar tissue might cause tightness or pulling sensations, leading to discomfort or pain, especially when moving the jaw.
Surgical site swelling
Swelling after parotid gland surgery is a normal part of the healing process but can result in jaw pain due to increased pressure on surrounding tissues.
Concerned about your recovery? Schedule a consultation with a specialist today.
Potential complications associated with jaw pain after parotidectomy
While jaw pain after parotidectomy is common and often resolves with time, there are potential complications that can arise if the pain persists or is linked to underlying issues:
Facial nerve weakness or paralysis
Chronic pain
Trismus (Lockjaw)
Frey’s Syndrome
Hematoma or seroma formation
Infection
Don’t wait—get expert advice on managing your post-surgery symptoms.
How to manage jaw pain after parotidectomy?

Managing jaw pain after a parotidectomy involves a combination of medical treatments, home care, and lifestyle adjustments. Here are some effective strategies to help alleviate the discomfort:
Medications:
- Pain relievers: Over-the-counter options like ibuprofen or acetaminophen.
- Prescription medications: If the pain is severe, your doctor may prescribe stronger painkillers or nerve pain medications
Physical therapy:
- Jaw exercises: To improve mobility and reduce stiffness.
- Massage therapy: To ease muscle tension and enhance blood flow.
Cold and warm compresses:
- Cold compresses: For reducing initial swelling and numbing pain.
- Warm compresses: To relax tight muscles and improve blood flow after the first few days.
Dietary adjustments:
- Soft foods: To minimize stress on the jaw and avoid aggravating pain.
- Small, frequent meals: To reduce the strain on the jaw during eating.
Oral Hygiene:
- Gentle brushing: To prevent infection and avoid irritation of the surgical area.
- Saltwater rinses: To keep the area clean and reduce inflammation.
Managing specific conditions:
- First bite syndrome: May be treated with medications such as botulinum toxin injections to reduce pain during eating.
- Trismus (Lockjaw): Physical therapy and stretching exercises can help improve jaw movement.
Surgical or medical interventions:
- Drainage: If there is significant fluid accumulation or a hematoma.
- Further surgery: In rare cases, additional surgery may be needed to address complications.
Follow-up care:
- Regular check-ups: To monitor recovery and adjust treatment plans as needed.
- Specialist referrals: For issues like chronic pain or significant functional impairment.
When to consult a surgeon?

- Pain persistence
If jaw pain continues despite treatment or worsens, it is important to get a professional evaluation. - Unusual symptoms
Seek advice if you experience unusual symptoms, such as new numbness or facial weakness. - Difficulty with jaw movement
If you have trouble opening your mouth fully or experience significant stiffness consult your surgeon. - Signs of infection
Persistent redness, swelling, or fever could indicate an infection that needs medical attention. - No improvement in function
If there’s no improvement in your ability to eat, speak, or perform daily activities, follow up with your surgeon.
Ready to take the next step? Book an appointment with a specialist now.
Conclusion
While jaw pain after parotidectomy can be an unsettling aspect of recovery, understanding its potential triggers and staying proactive in your care can make a significant difference. It is important to approach your healing process with patience and the right support. Should any concerns arise, consulting an expert like Dr. Devendra Chaukar ensures you access specialized care tailored to your needs. With the proper attention and guidance, most patients find relief and can move forward confidently in their recovery journey.
Frequently Asked Questions:
How long does jaw pain last after surgery?
Jaw pain after parotidectomy usually lasts a few weeks, but it can persist for several months in some cases. If it continues longer, consult your surgeon.
What is the aftercare for parotidectomy?
After a parotidectomy, keep the surgical site clean and dry, manage pain with medication and cold compresses, follow a soft diet, and attend follow-up appointments with your surgeon.
Facial exercises after parotidectomy
What is first bite syndrome after parotidectomy?
First bite syndrome is an intense, sharp pain in the jaw or temple area during the first few bites of each meal after parotidectomy, caused by nerve disruption from the surgery.
Disclaimer: The information shared in this content is for educational purposes only and not for promotional use.

Dr Devendra Chaukar
Dr. Devendra Chaukar is a renowned Head and Neck Surgical Oncologist with over 20 years of experience in treating complex head and neck cancers. A graduate of Tata Memorial Hospital, Mumbai, he specializes in minimally invasive surgeries and organ-preserving treatments. Dr. Chaukar is deeply committed to patient-centric care and advancing cancer treatment through research and education.

Recent Comments